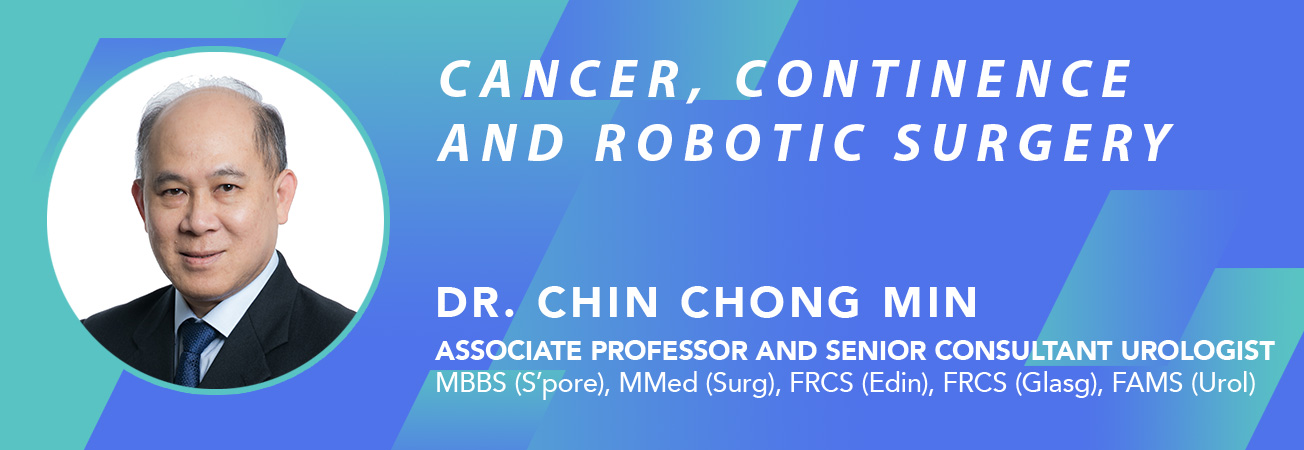
Flexible Cystoscopy

This procedure is easily done under local anaesthesia. After anaesthetic gel is given via the urethra, a flexible scope smaller than the size of a pen is inserted into the bladder under direct vision. The procedure takes between 5 to 15 minutes. Slight bleeding and painful urination (dysuria) can be expected after the procedure, Bleeding is more likely to occur if a biopsy is taken. The blood in the urine and dysuria usually settles by the next day. Flexible cystoscopy itself is a short procedure and the risk of urine infection is low.
It is indicated in the following situations:
- Persistent or significant blood in the urine (haematuria)
- Bladder mass detected on ultrasound or xray
- Surveillance for recurrence of bladder cancer
- Recurrent bladder infections (UTI)
- Assess urethra in suspected stricture
- Assess prostate in men
- Removal of DJ stent
Haematuria
A scope in indicated for persistent haematuria as small bladder tumours < 1 cm may not be seen on ultrasound scans or xray. Flat tumours and ulcers are better appreciated from endoscopy, and the vision enhanced by the magnification on the monitor. At the same time, a biopsy can be taken to confirm if the bladder lesion is cancerous or benign. Although the urine can be sent for cytologic examination to look for cancer cells, its accuracy is limited by low sensitivity (< 50% pick-up rate). Hence, cytology result is not to be relied on when deciding whether haematuria is due to cancer or not.
Bladder mass

Bladder tumour shown on ultrasound
Bladder masses are sometimes reported during ultrasound screening. If so, endoscopy is the best way of seeing if it is cancerous or not because a biopsy can be taken during the scope. Sometimes, the ultrasound or xray scan may over-report a lesion. Direct visualisation is the best way of confirming what this lesion is.
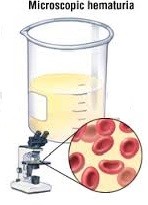
Surveillance for recurrent bladder cancer
Small, flat bladder cancer recurrence cannot be seen on ultrasound
Following resection of bladder cancer (TURBT), surveillance scopes are still needed as part of the follow-up protocol because the chance of cancer recurrence is as high as 80%. The standard regime is every 3 months for the first year and 6 monthly for subsequent years so as to detect any early recurrence. Such recurrent tumours will be small and not visible on ultrasound. It is important to detect any small recurrences as they can be ablated at the same time using a diathermy probe.
Recurrent UTIs
Women are especially prone to bladder infections despite good hygiene and drinking adequate water or cranberry juice. On the other hand, if the urine culture is persistently negative but dysuria is still felt, the cause may be a chronic inflamed urethra (urethritis). Only a cystoscopy can confirm this. At the same time, the scope can assess the bladder for any occult cause that may mimic symptoms of infection..
In women who had previous sling surgery for stress incontinence, tape erosion into the bladder can occur many years later. as to be excluded. This tend to cause dysuria and recurrent UTIs or stone formation. Such tape erosions are best seen on cystoscopy because even a CT scan will not show such foreign body.

Tape erosion into the bladder neck after previous sling surgery
Urethra Stricture
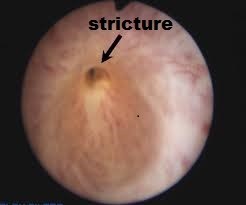
Pin-hole stricture in a male urethra
This occurs as a result of previous trauma to the urethra, e.g. after catheterization or endoscopic surgery like TURP. Whilst urine flow test (uroflow) may help diagnose the stricture, the degree and severity of the stricture may not be easily appreciated, even with xray study (urethrogram). The flexible cystoscopy gives visual appreciation of how small the stricture is. At the same time, dilatation can be performed if the stricture is not too tight.
Prostate enlargement
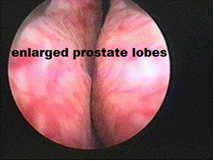
Occlusive BPH as seen on cystoscopy
Although BPH can be assessed from ultrasound, there are cases where the prostate size may not be large and yet, these men seem to have voiding difficulty. A cystoscopy can better appreciate the degree of bladder obstruction as it gives a visual assessment of the prostate lobes, bladder neck and bladder muscle. The scope will also show if there is any inflammation of the prostate (prostatitis) contributing to dysuria.
Remove DJ stent
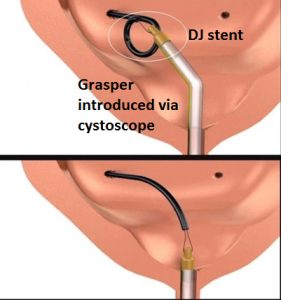
DJ stent in bladder removed via the flexible cystoscope
A DJ stent is often inserted during stone or kidney surgery. This stent cannot be left in for too long and needs to be removed. This is easily done through the flexible scope using a long flexible grasping forceps. Some pain along the urethra is to be expected as the stent is being pulled out.

Dr Chin doing flexible cystoscopy under local anaesthesia in a male patient
Complications include:
- Dysuria (transient)
- Bleeding if a biopsy taken or large BPH with prostatitis is present
- UTI ( < 1% )