Urinary Incontinence
5 Key points:
- There are many causes of urinary incontinence even though the history may seem similar
- It is important to arrive at the right type of incontinence and this requires a specialist who is trained in bladder dysfunction
- A proper physical examination, lab and urodynamic investigations will help differentiate the types of incontinence
- Treatment success is very much dependent on a clear understanding of the anatomic and neurophysiological defect
- Should surgery be required, it is important to get the surgery right the first time, because repeat surgery gives poorer success rates
Urinary incontinence is the uncontrolled leakage of urine from the bladder. There are many types of incontinence and before treatment can be advised, one must be clear of the type of incontinence and its underlying cause. Incontinence affects one’s quality of life and even though it tends to be age-related, it can still be corrected in most cases.
Evaluation
This is assessed from the history, physical examination and relevant lab or xray investigations. Sometimes, urodynamic tests may be needed; this is the study of the bladder and urethra function by means of a machine connected with tubes and electrodes inserted into the bladder and rectum [Fig 1].
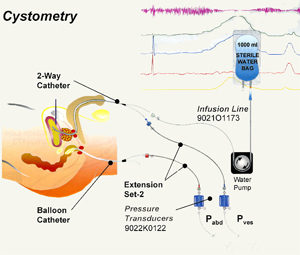
Fig 1. Urodynamics can help determine the type of incontinence, especially in complicated cases.
Types & Treatment

There are 4 types of incontinence:
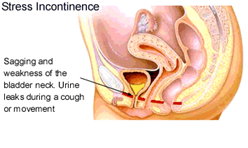
1. Stress Incontinence [Fig2].
This type of incontinence affects mostly women and occurs upon physical exertion, e.g. carrying loads, coughing, and sneezing. It is due to weak pelvic floor muscles following traumatic childbirth, menopause or pelvic surgery [Fig 2]. It can also occur in men following prostate surgery. The treatment is initially physiotherapy, e.g. pelvic floor exercises in which one squeezes these muscles frequently and repeatedly. However, up to one-third of sufferers cannot do this exercise. If so, then surgery to restore the bladder support is needed.
There are many types of surgery to correct stress leak, ranging from open surgery (colposuspension) to minimally-invasive sling surgery to bulking agent injection. The most popular surgical method is sling surgery because it is minimally-invasive, has high cure rates with minimal complications. Sling surgery can be done as a day case with quicker return to normal activities. The most popular sling is the TVT (tension-free vaginal tape) which is placed under the middle part of the urethra. The surgery takes 30 mins and the cure rate is > 90%. Complications include bladder injury during its insertion and voiding difficulty if the tape is placed too tight. Late complications include tape erosion into the bladder or vagina. Hence, although it is a “ simple “ surgery, it still requires a surgeon who has undergone proper training. A variant of the TVT surgery is the TOT in which the tape exits through the side of the thigh rather than through the top. [Fig 3].
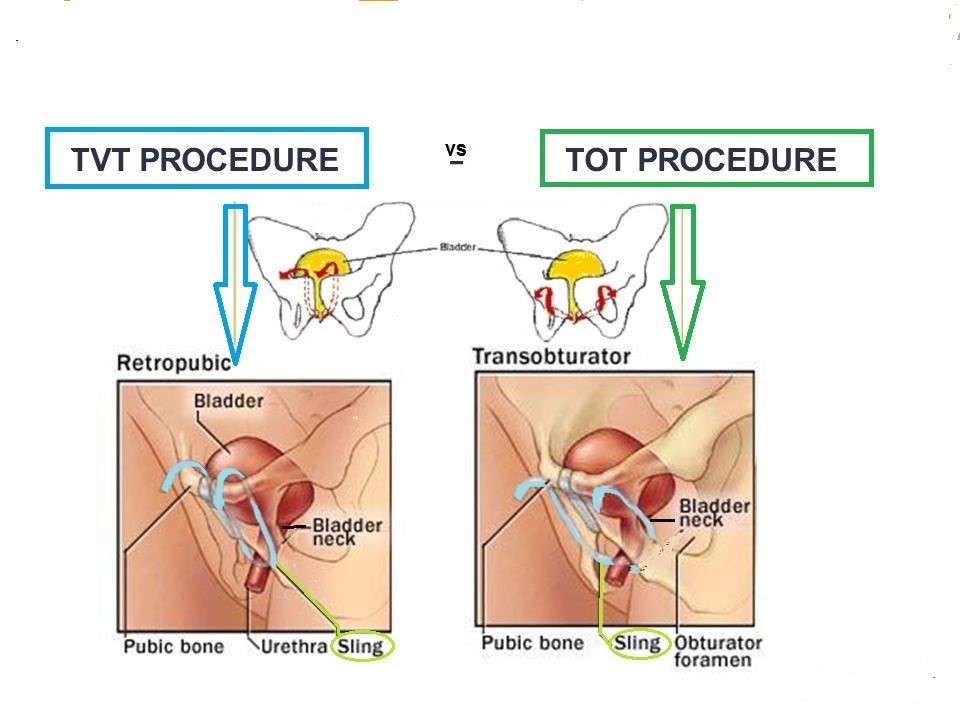
Fig 3. TVT and TOT uses a polypropylene tape placed under the mid-urethra; the difference being the direction of the sling support
Bulking agent injection into the bladder neck is an alternative method, especially in frail elderly women. The agents injected range from collagen to silicon particles. The advantage is that this is an even simpler procedure that can be done under local anaesthesia. The disadvantage is that repeat injections are usually needed.
In men, the most common cause is post-prostatectomy after prostate cancer surgery. A male sling is now available to correct persistent stress leak [Fig 4].
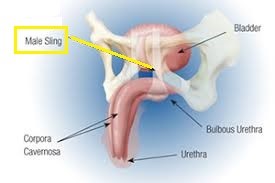
Fig 4. A sling can be placed under the bulbous urethra to correct stress incontinence in men
2. Urge Incontinence
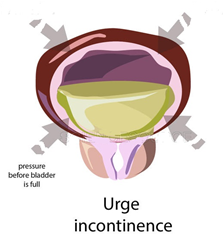
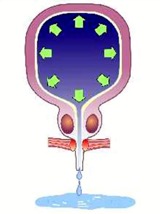
This is leakage of urine as a result of an overactive bladder (OAB). OAB occurs in up to 15% of the population. In severe cases, the strong sense of urge is difficult to control so much so that leakage occurs even before reaching the toilet. Urge incontinence can usually be controlled by medication e.g. oxybutynin, tolterodine, solifenacin, mirabegron. They work by inhibiting the bladder contractions [Fig 5].
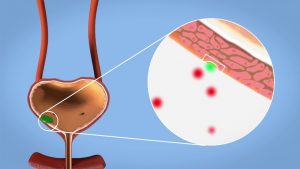
Fig 5. Drugs for urge incontinence work by inhibiting bladder contraction
Some patients cannot tolerate the side-effects, esp. dry mouth, dry throat, dry skin, constipation. In such a situation, surgical methods can be considered, e.g. botox injection of the bladder [Fig 6], or neuromodulation.
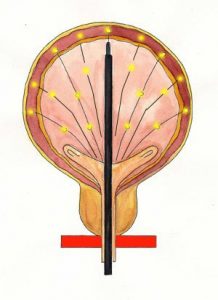
Fig 6. Botox can be injected into the bladder for refractory urge incontinence cases
3. Overflow Incontinence
This is the leakage of urine from chronically full bladders due to long-standing blockage e.g. from an enlarged prostate (BPH) or weak bladder muscles, e.g. in elderly, diabetics. [Fig 7]. The leak typically occurs upon getting up from a lying position or upon straining and can be difficult to distinguish from stress incontinence. This incontinence is suspected when one finds a distended bladder on examining the abdomen. Urodynamics can confirm this type of incontinence. In the case of overflow incontinence form a weak bladder muscle, treatment consist of a cholinergic drug e.g. Ubretid or by self-catheterisation using a soft silicon catheter. If a BPH is found, then prostate surgery (TURP) is recommended.
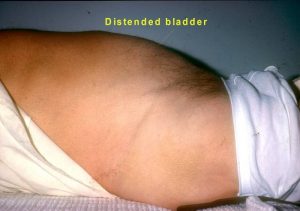
Fig 7. Overflow incontinence due to chronic retention from enlarged prostate
2. Total Incontinence
This occurs after surgical damage to the urethral sphincter muscle, esp. after prostate and major pelvic surgery. The urine continually leaks out. The only solution to correct this is to implant an artificial urinary sphincter. This is a major procedure which takes 4 to 5 hours. An inflatable cuff is placed around the bladder neck or urethra. To empty the bladder, the button controlling this cuff is pressed, resulting in temporary deflation of this cuff [Fig 8]. The most common complications are malfunction and infection of the device.
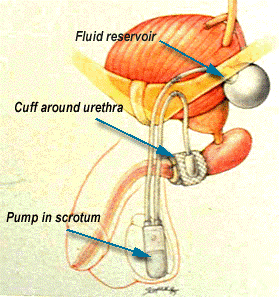
Fig 8. The artificial urinary sphincter controls total incontinence through an inflatable cuff placed around the urethra
Summary
There are many types of urinary incontinence. It is important to categorise the type of incontinence and understand the pathologic mechanism before correct treatment can be given. If corrective surgery is needed, it is crucial that it is performed by experienced surgeons as the success rate for re-do surgery is poorer.