Prostate Cancer
5 Key Points:
- Prostate cancer is now detected at an early stage as a result of health screening
- The diagnosis is suspected when the PSA is > 4 ug/L and confirmed from prostate biopsies
- MRI can be done prior to biopsy to look for suspicious areas and facilitate fusion biopsy
- Treatment choices vary from active surveillance, surgery to radiotherapy.
- Surgery still gives the best cure rate ( > 90% cure ) and the robotic method is now the preferred choice because of faster recovery of continence, better preservation of potency and lower chance of leaving cancer behind
Prostate cancer is very rare before the age of 50 years. Most cases are detected in men above 60 years old. Genetic causes account for only 9% of cases. From migration studies, a high fat diet seems to be the common risk factor. Prostate Cancer is now the top cancer in Singapore men. The general consensus that this is predominantly a disease of the Western world may not be true anymore. Although epidemiological studies show a wide difference in the incidence between Western and Asian populations, with the fast ageing population and westernised diet, prostate cancer has become more common in Asian men.
Symptoms
In its early stages, prostate cancer does not cause any symptoms. As the cancer progresses, the enlarging tumour compress the urethra, blocking the flow of urine. When this happens, frequent urination and terminal dribbling occur. Occasionally, blood in the urine or semen is the first sign of prostate cancer. As prostate cancer advances, it spreads to the pelvic lymph nodes and the bones to cause bone pain and even fractures. A late manifestation is spinal cord compression and paralysis.
Stages
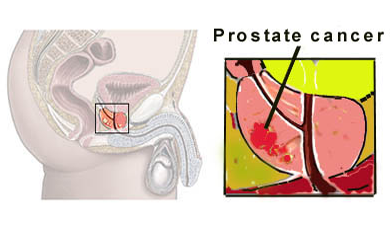
Prostate Cancer is classified into its 4 stages [Fig 1].

Figure 1. Stages of Prostate Cancer
In Stage 1, there are no symptoms. The cancer is small volume and cannot be felt with the finger. It is diagnosed at health screening when a high PSA level (> 4 ng/dl) is found.
In Stage 2, prostate cancer can be felt as a hard nodule on rectal examination. Although the cancer is bigger, it is still confined within the prostate and cure still possible.
By Stage 3, the cancer has spread out of the prostate capsule. Common symptoms at this stage include difficult urination. This is now at locally advanced stage and carries a lower chance of cure. Treatment is aimed at slowing its spread and preventing bladder blockage. The PSA level is usually > 10 ng/dl at this stage.
At Stage 4, the cancer has already spread beyond the prostate to the lymph nodes and bones. Symptoms at this stage include difficult urination, bone pain, weight loss and fatigue. At this stage, treatment is targeted at preventing further complications and reducing pain. The PSA level is usually > 100 ng/dl by now.
Diagnosis
The most reliable method of diagnosing prostate cancer is a biopsy. This is usually done via the rectum under ultrasound guidance (TRUS) [Fig 2]. Because this procedure carries the risk of infection and bleeding, prophylactic antibiotics are given to reduce this risk to < 5%. Anti-platelet drugs like aspirin and plavix must also be stopped prior to biopsy. It is now standard practice to take at least 12 cores. To reduce pain during the biopsy, local anaesthesia is given via a peri-prostatic nerve block.
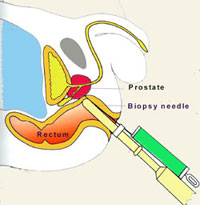
Fig 2. Prostate biopsy via transrectal ultrasound guidance
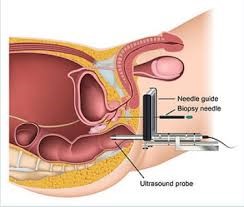
To reduce the risk of infection, the transperineal route can be attempted [Fig 3]. But this requires sedation in addition to local anaesthesia and a different set of biopsy equipment.
The accuracy rate for ultrasound guided biopsy is in the range of 80%. Multiparametric MRI (mpMRI) is now done prior to biopsy to image any suspicious cancer areas [Fig 4]. The radiologist assigns a PIRADS score to the lesion and a score of 3,4 or 5 is suspicious enough to be biopsied.
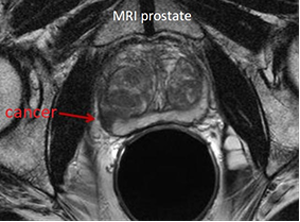

Fig 4. MRI showing a cancerous area
The mpMRI also facilitates ultrasound-fusion method to improve the biopsy accuracy rate to 99% [Fig 5].
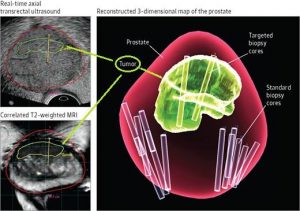
Fig 5. Multiparametric MRI – ultrasound fusion biopsy technique
Obtaining a biopsy is important because the histological grading also determines the risk and rate of cancer spread. This is the Gleason score and a score of 8 to 10 indicates a fast-growing cancer with a high risk of spread and death [Fig 6].
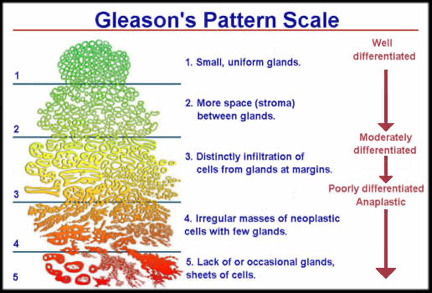
Fig 6. Gleason scoring for prostate cancer
The Gleason score is important as it also helps to stratify the risk of cancer progression taking into consideration the pre-biopsy PSA level and the clinical stage [Fig 7].
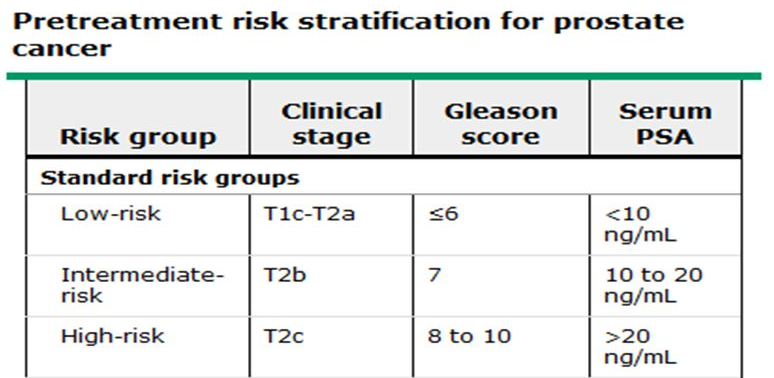
Fig 7. Risk stratification for prostate cancer
After confirmation of cancer, a Bone scan [Fig 8] or PSMA PET CT scan [Fig 9] is done to see if the cancer has spread out of the prostate.

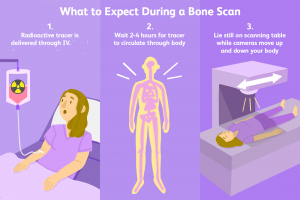
Fig 8. Bone scan to detect any spread to the bones
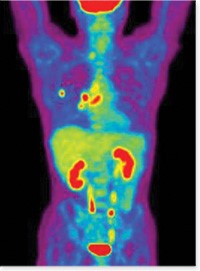
Fig 9. PSMA PET CT to specifically detect prostate cancer in the whole body
The PET CT scan is expensive and best reserved for high-risk cases and for biochemical failure cases, i.e. rebound of PSA after treatment to above 0.4 ug/L with the aim to locate where the recurrence.
Treatment
Early Prostate Cancer (Stage 1 & 2)
When the tumour is limited to the prostate gland, the cure remains high (> 90% survival). This is achieved through surgery or radiation, but advocated only for men who are expected to have a life-span of 10 years or more.
- a) Surgery (Radical Prostatectomy)
Here, the entire prostate containing the tumor is removed [Fig 10]. Pelvic lymph nodes are also sampled if the PSA is > 10 ug/L or the tumour is of high-grade. Complications include excess bleeding, urine leak, impotence and incontinence. A relatively young, otherwise healthy man is an ideal candidate for surgery. The laparoscopic technique is a minimal invasive method of doing radical prostatectomy with the advantage of less pain and faster recovery, but the robotic method is now the gold-standard because of minimal blood loss and better functional outcomes, thanks to the 3-dimentional, magnified vision and articulate robotic arms which help the surgeon to spare the erectile nerves and achieve a water-tight anastomosis of the bladder to the urethra.
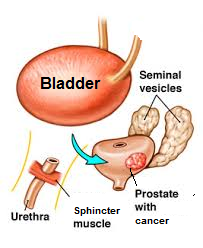
Fig 10. Radical prostatectomy is the removal of the entire prostate gland
b) Radiation (External beam or Brachytherapy)
Radiation therapy uses high energy X-rays to kill the cancerous cells. There are 2 ways to administer this therapy, either externally (DXT) or internally (brachytherapy). External beam is a daily session lasting 7 weeks. Side-effects include fatigue, skin reaction, frequent urination, diarrhoea and rectal bleeding. Brachytherapy is a 2-step process that involves planting multiple radioactive seeds within the prostate after soft-ware imaging and planning. This is to ensure accurate placement to cover the whole prostate and minimise seed expulsion out of the urethra [Fig 11]. Long term side effects of radiotherapy are cumulative and include radiation cystitis (bleeding), urinary / faecal incontinence and impotence.
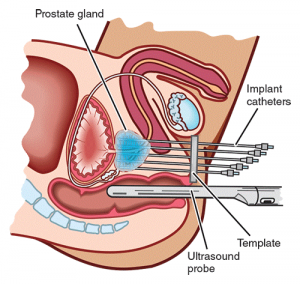
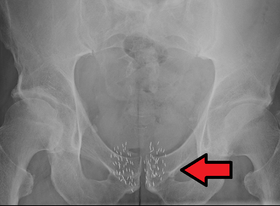
Fig 11. Brachytherapy where radioactive seeds are implanted into the prostate
Radiotherapy is often combined with hormonal treatment to achieve better response rates. The limitation with radiotherapy is that high-grade cancers may not be destroyed and the cure rate not as durable as surgery. However, its appeal is the avoidance of surgery-related risks. For this reason, it is suited for older men and those with multiple medical problems.
c) High-Intensity Focused Ultrasound (HIFU) & Cryotherapy
These two modalities employ high energy to destroy the cancer area in the prostate; HIFU through heat [Fig 12a] and Cryotherapy though freezing [Fig 12b]. However, they are best reserved for small volume, localized, low-grade cancers as the whole prostate is not treated. The limitation is the recurrence rate is as high as 20% and cancer can still develop in the non-treated areas. Also, the PSA level will not drop to < 0.1 ug/L as most of the prostate gland is not treated. As the long-term cure rate is not known, these alternative methods are best done in a trial setting.
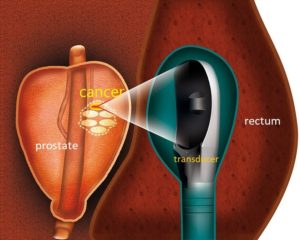
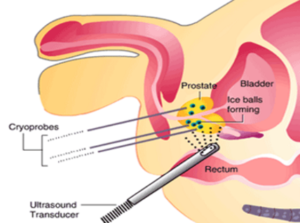
Fig 12a. HIFU uses focused ultrasound
Fig 12b. Cryotherapy to freeze the cancer
d) Active Surveillance
Active surveillance (AS) is an option based on autopsy studies which showed that many men who died of other illnesses harboured prostate cancer. AS is feasible for older men (above 75 years) and those with low-grade, low-volume prostate cancer. The problem with adopting this policy is that as much as 30% of such cancers do progress to aggressive cancers and ultimately require intervention. AS is not suitable for men who are anxious about the risk of progression; indeed, many men opt out of AS when they see their PSA continue to climb.
Advanced Prostate Cancer (Stage 3 & 4)
Both surgery and radiation can still be used either alone or together to treat Stage 3 disease. However, most Stage 3 cancers will also require hormonal treatment to suppress the cancer cell growth.
In Stage 4, palliation is the only option and aimed at depleting the testosterone level. (castration). Control of the disease is achieved by either reducing the production of testosterone, the hormone that fuels the cancer, or blocking its action. Depriving prostate cancer of testosterone causes it to shrink and this is achieved in one of 3 ways:
a) Orchidectomy
This is the surgical removal of the testicles and is a minor operation. As 95% of testosterone is produced by the testes, orchidectomy immediately brings down the testosterone levels to zero, thereby, inhibiting cancer growth.
b) Anti – Androgens
These drugs block the action of testosterone on the cancer cell. There are many new drugs now. Side-effects vary from diarrhoea to painful breast enlargement (gynaecomastia). They are costly and have to be taken daily without interruption.
c) LHRH analogs
This group of drugs is given by injection under the skin at 1 or 3 monthly intervals [Fig 13]. They act by depleting testosterone production from the testicles, similar to orchidectomy.

Fig 13. Injection of LHRH drug under the skin
For painful bone involvement, direct radiation to the bone or biphosphonate drug infusion eg. Zometa, can be given to halt further bony destruction. Because advanced prostate cancer causes excess pain and morbidity once it spreads to the bones, early detection is still the best way to prevent such excess suffering. Because of advancements in medical therapies, men with advanced cancer are now living longer. However, the lifetime cost will be higher than treatment for organ-confined cancer.
For painful bone involvement, direct radiation to the bone or biphosphonate drug infusion eg. Zometa, can be given to halt further bony destruction. Because advanced prostate cancer causes excess pain and morbidity once it spreads to the bones, early detection is still the best way to prevent such excess suffering. Because of advancements in medical therapies, men with advanced cancer are now living longer. However, the lifetime cost will be higher than treatment for organ-confined cancer.
Summary
Prostate cancer is more common as men age. Excess morbidity results when it is diagnosed late. Fortunately, there is a tumour marker, PSA which can detect the cancer in its early stages. PSA also serves as a surrogate marker for effectiveness of treatment and alert to any recurrence. The threshold for biopsy is 4 ng/dl but majority of men with high PSA do not have prostate cancer. Biopsy is recommended when the PSA is consistently high and continues to rise. This can be done via the rectum or perineum. Prior to biopsy, a MRI is now routinely done with the advantage of reducing the need for unnecessary biopsies as well as improving the accuracy rate through fusion with the ultrasound image. Upon confirmation of organ-confined cancer, surgery still gives the most reliable long-term survival, the gold-standard method being robotic prostatectomy.