Overactive Bladder

5 Key points:
- Symptoms are urgency, frequency and even urge incontinence
- Triggers are cold weather, caffeine drinks, hearing sound of water and mental stress
- Diagnosis is made by exclusion of urine infection, bladder lesions and nerve disorders
- Drugs are most effective and require at least 3 to 6 months to “re-set” the bladder
- Effectiveness of medication is limited by their side-effects, esp. dry mouth, dry eyes, dry skin, drowsiness and constipation
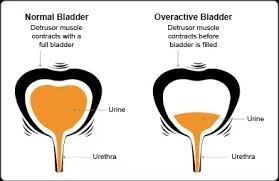
Patients who suffer from overactive bladder (OAB) complain of frequent urination both day and night. They often experience strong urge to urinate at inconvenient and unpredictable times and may even leak urine before reaching a toilet (urge incontinence). This causes embarrassment, poor self-esteem and affect their quality of life.
Overactive bladder afflicts men and women equally. Some 15% of the population suffer from OAB, the prevalence being higher in older patients. The cause is unknown, but common aggravating factors include excess caffeine intake, cold weather and mental stress. Elderly men with prostate enlargement (BPH) also tend to develop OAB symptoms.
Diagnosis
The diagnosis of OAB is made after excluding underlying causes such as:
- Bladder infection (UTI)
- Bladder stones
- Drug side-effects
- Neurological disease (e.g. Parkinson’s disease, stroke, spinal cord lesions)
- Nerve damage from pelvic trauma or surgery
- Bladder or prostate cancer
A complete medical history is taken, including a bladder diary [Fig 1], physical examination, and urine analysis. Examination of the urine may identify bacteria (indicating infection) and excess sugar (indicating diabetes mellitus). If blood is detected, a flexible cystoscopy may be needed to exclude bladder cancer. Occasionally, other diagnostic procedures like urodynamics are needed if there is no response to medical measures.
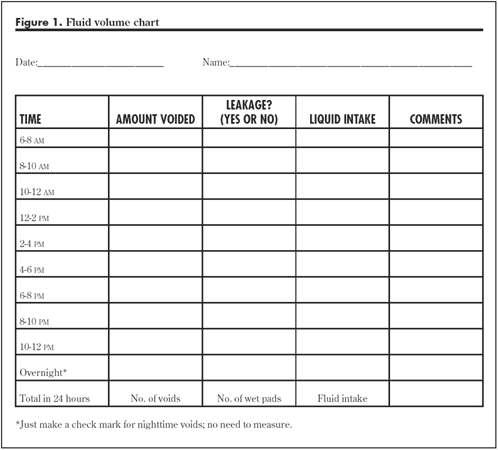
Fig 1.Bladder diary to record fluid intake, number of toilet visits & leak episodes
Treatment
Treatment is step-wise and proceeds in the following order:
- Behaviour modification and Bladder training
- Medication
- Botox injection
- Neuromodulation
- Surgery
1) Behaviour modification and Bladder Training
The first step is identifying and correcting habits that aggravate this condition eg. excess water / coffee drinking. Self-help advice e.g. bladder training and Kegel exercises may also help reduce the sensation and delay urination. This is often done in conjunction with a bladder diary.
2) Medication
Many drugs are available and are very effective. These medications work by relaxing the muscle of the bladder and reduce their contractions. The most commonly prescribed drugs are tolterodine (Detrusitol®), oxybutynin (Ditropan®), trospium chloride (Spasmolyt®), propiverine (Mictonorm®), and solifenacin (Vesicare®). These tablets are taken once to twice a day and the effect is seen by 2 weeks. Up to 80% of patients are cured by 3 to 6 months of medication, although there will be those who need to be on these drugs long term.
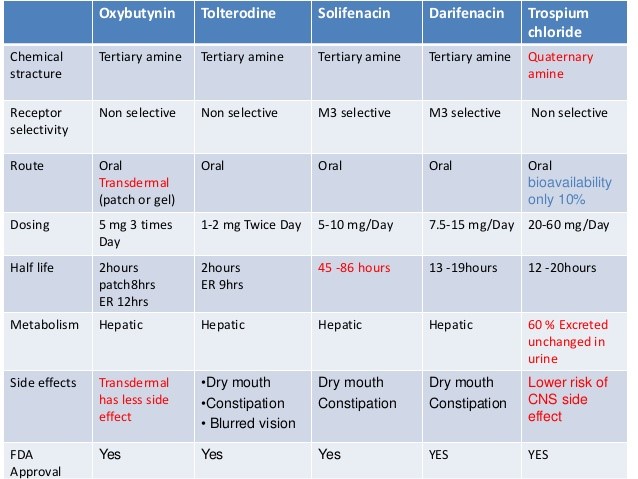
Differences between the various anti-muscarinic drug
The main limitation to medications is their side-effects, especially dry mouth, dry eyes, constipation, headache, blurr vision, drowsiness, and urinary retention. This can be experienced in up to 30% of patients. These drugs are contraindicated in those who have narrow-angle glaucoma. The latest drug, mirabegron (Betmiga®) acts on a different category of receptors without the side-effect of dryness of mouth, eyes and skin.
3) Botox injections
Botox can be injected into the bladder for those who do not respond to oral medication [Fig 2]. About 100 to 150 units of botox is injected into the wall of the bladder to paralyze the bladder muscle and suppress their contraction. The effect is seen as early as 2 weeks after injection. This procedure is normally done as a day case under general anaesthesia and takes 15 mins to do. Success rates vary from 50% to 70% but the effect last 6 to 9 months. Repeat injections may then be needed. Complications include bloody urine and retention of urine that may require self-catheterisation.
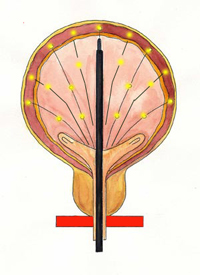
Fig 2. Botox can be injected into the bladder for severe cases
4) Neuromodulation (Sacral Nerve Stimulation)
This is reserved for those who fail medication and botox bladder injection. It requires a special device and is an expensive procedure. It consists of a neurostimulation device system that sends mild electrical pulses to the sacral nerve at regular intervals to modulate it. As it may not work for all patients, a trial electrode is first implanted into the sacrum [Fig 3]. This wired electrode is tested with an external meter over a period of 3 to 5 days as the patient records voiding patterns that occur with stimulation. The record is compared to recorded voiding patterns without stimulation. The comparison demonstrates whether the device will effectively reduce symptoms. If the test is successful, the neurostimulator device is then implanted under the skin at the level of the upper buttock. The most common complications are infection and breakage of the device / wire.
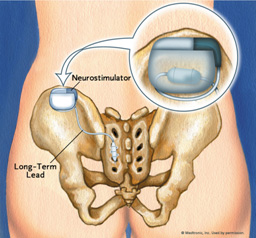
Fig 3. Neuromodulation of the bladder through sacral nerve stimulation
5) Surgery (Augmentation Cystoplasty)
If all else fails, surgery to enlarge the bladder will work. It involves splitting the bladder and patching a segment of small intestine onto it [Fig 4]. This is a major undertaking and irreversible, hence, patients must be aware of possible complications like mucus blockage of the bladder, incomplete bladder emptying, night-time incontinence and UTIs.

Fig 4. Augmentation cystoplasty where the bladder is enlarged by patching a segment of small intestine over it
Summary
Overactive bladder is a functional disorder of the bladder which is diagnosed after excluding other causes. It tends to be age-related. Medications are the most effective in controlling this disease, the limitation being the side-effects. Botox injections into the bladder is the next-line and reserved for non-responders and those with urge incontinence.