Male Infertility
5 Key points:
- Male infertility can be due to congenital or acquired factors
- Evaluation requires semen analysis, hormonal profile and scrotal ultrasound, of which the only correctable factors are hormonal, obstructed vas and varicocoeles
- Varicocoele as the cause of subfertility should be bilateral in nature
- Azoospermia is often due to genetic absence of sperm-producing cells in the testis, blockage or absence the vas or retrograde ejaculation
- Ultimately, the subfertile couple may have to resort to IVF if the sperm quantity and quality cannot be improved
The male factor as a cause for subfertility is suspected when the couple has tried for more than 1 year and the wife has been evaluated to have normal reproductive organs and regular cycles. In 50% of these infertile couples, investigations will reveal a pathology in the woman alone. In another 20%, the abnormality lies in both the man and woman. In the remaining 30%, the problem lies in the husband.
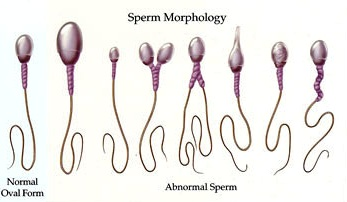
Conception requires fertilisation of a healthy egg by a healthy sperm. This requires the timely release of the ovum and deposition of semen in the vagina. The chance of any spermatozoa reaching the ovum is a function of their quantity, quality and the ability to penetrate the egg. Evaluation of the infertile couple should therefore involve the couple from the outset until an abnormality is uncovered. An abnormal sperm count is usually the earliest indicator of a male factor.
The production of spermatozoa requires normal levels of sex hormones. Production of sex hormones is principally regulated by the pituitary gland of the brain. Conditions that affect the pituitary gland may result in infertility, sometimes with impotence too. Other causes of hormone imbalance include liver disease and steroid medications. Defective spermatozoa production can also occur without any apparent hormonal imbalance. Many of these cases are due to genetic disorders.
Causes
- Congenital / Genetic. Chromosomal defects like Klinefelter’s syndrome, Noonan’s syndrome, congenital adrenal hyperplasia and absent testes are congenital causes. Undescended testes tend to be functionally defective and poor producers of spermatozoa.
- Acquired. Sperm production can be affected by previous chemotherapy, radiotherapy, certain medications (cimetidine, spironolactone, ketoconazole), cigarette smoking and excess alcohol consumption. Spermatozoa production takes place in the testes at a temperature 1 degree C below normal body temperature. Childhood mumps can cause severe testicular damage when both testicles are infected. Varicocoele, a condition of dilated, tortuous spermatic veins within the scrotum, is also a common cause for subfertility, possibly because of venous congestion and higher temperatures on the testis [Fig 1].

Fig 1. Varicocoele is the collection of dilated veins in the scrotum. This tends to raise the temperature within the testicle and decrease sperm production
Azoospermia (zero sperm count) is an even severe form of subfertility and can be due to absent sperm-producing cells (Sertoli only cell syndrome), retrograde ejaculation of semen into the bladder, or blocked / absent vas [Fig 2]. Varicocoeles do not cause azoospermia.
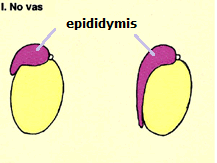
Fig 2. Absent vas as a cause of azoopermia
Evaluation
After the history taking, a general physical and scrotum examination is done. Blood test for hormone levels and a semen analysis is done next. Majority of male subfertility are of low number/quality as a result of impaired sperm production from genetic defect in the Y chromosome. A low semen volume with azoospermia suggests a blocked vas while an inadequate concentration of spermatozoa suggests impaired production. Small, poorly developed testes indicate primary testicular failure while azoospermia in the presence of normal testes suggests an obstructed or absent vas.
If blockage of the vas is suspected, a transrectal ultrasound scan of the seminal vesicles and ejaculatory duct will show distended and dilated seminal vesicles. Ultimately, the best way to sort out azoospermia is surgical exploration of the testes which includes testis biopsy, vasography and sperm retrieval from the epididymis / testis. Any harvested mature sperms is frozen for future assisted reproduction. If obstruction is the root cause, corrective surgery can be done to relieve the blockage.
Management
Treatment can only be initiated after clinical assessment and laboratory investigations are completed. The couple will be advised on possible corrective procedures and whether to go on to costly assisted conception techniques.
- Medication
If the hormonal assays are normal, then supplements eg. vitamins A, C and E may be tried for a few months. Lifestyle changes, especially smoking, alcohol drinking are also advised. If the fertility-related hormones are low, a synthetic oral fertility hormone, e.g. clomiphene can boost the levels. It is not correct to give testosterone supplements if the testosterone level is low because the excess testosterone will cause negative-feedback regulation on the pituitary gland.
- Varicocoele ligation [Fig 3]
If varicocoele is the only identifiable factor found, most urologists would advise surgery to ligate these big veins. However, the varicocoele ought to be obvious clinically and present on both sides of the scrotum based on independent ultrasound assessment. Assuming that the ligation is complete with no recurrence, the semen quality should improve by 6 months. If not, then the more likely cause is an underlying genetic defect of the sperm producing cells.


Fig 3. Site for varicocoele ligation. It is best to use the operating microscope to avoid accidental injury to the testicle artery
- Exploration of the scrotum
This is indicated if obstruction is suspected or when the cause of absent spermatozoa is in doubt. Vasography is done to rule out obstruction. Corrective procedures can subsequently be carried out to unblock the site of obstruction. The testis is also biopsied to assess the status of sperm production. Sperm retrieval is carried out next and any motile, mature sperms found are stored and frozen.
- Surgery for obstructed ejaculatory duct
If the ejaculatory ducts are blocked at its opening into the urethra, they can be opened through transurethral resection (called TURED). A resectoscope is inserted via the urethra and the opening of the ejaculatory ducts incised. This surgery is technically not easy to perform and the duct can be re-blocked by excess scarring.
Retrograde ejaculation is more difficult to treat. The sperms are retrieved from the urine voided immediately after ejaculation. The urine needs to be rendered alkaline to prevent the fragile sperms from dying.
Modern fertility centres offer a variety of assisted conception techniques including procedures such as in vitro fertilisation (IVF), gamete intrafallopian transfer (GIFT) and intracytoplasmic sperm injection (ICSI) – where a single spermatozoon is injected into the egg to boost the conception rate [Fig 4].
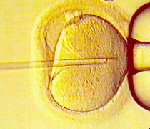
Fig 4. ICSI. A single sperm is injected directly into the egg to improve the chance of fertilization as compared to IVF
Summary
The approach to male infertility requires a systemic evaluation through physical examination, scrotal ultrasound, hormonal and semen analysis. The aim is to identify reversible factors before resorting to artificial means of conception which are expensive and stressful to the couple.