Benign Prostatic Hyperplasia (BPH)
5 Key points:
- BPH usually begins at the age of 50 years
- The initial symptoms are that of frequent urination both day and night, followed by difficulty and dribbling at end of the stream
- If untreated, the enlarged prostate can lead to painful acute retention of urine and obstructed kidneys
- Medication is the first-line treatment and effective in up to 80% of cases
- Some 15% of patients will still fail medication and will need surgery, the gold standard being TURP
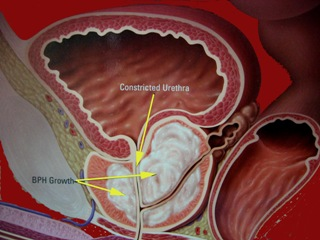
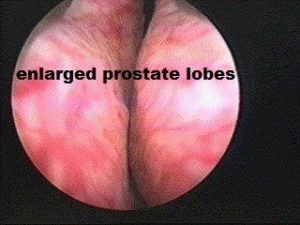
BPH is the benign enlargement of the prostate. The prostate gland is a small organ the size of a walnut that sits just below the bladder and surrounds the urethra. It produces fluid for nourishment of sperms. However, after the age of 50 years, it tends to enlarge due to hormone imbalance; BPH tends to obstruct and irritate the bladder, leading to symptoms like slow / intermittent stream, and urinary frequency both day and night. BPH is assessed from the history, physical examination, ultrasound and uroflow investigations. Left untreated, the consequences are: damage to the bladder, urine infections, bladder stones and even kidney failure. Many men mistaken the symptoms to be due to an ageing bladder, but an enlarged prostate (either from BPH or cancer) needs to be excluded before assuming that the bladder symptoms are just “part of ageing”.
Assessment:
1. International Prostate Symptom Score (IPSS) [Fig 1]. This is a questionnaire that covers the symptoms from the enlarging prostate. The total score gives an indication of the severity of the prostatic symptoms and how bothersome it is.
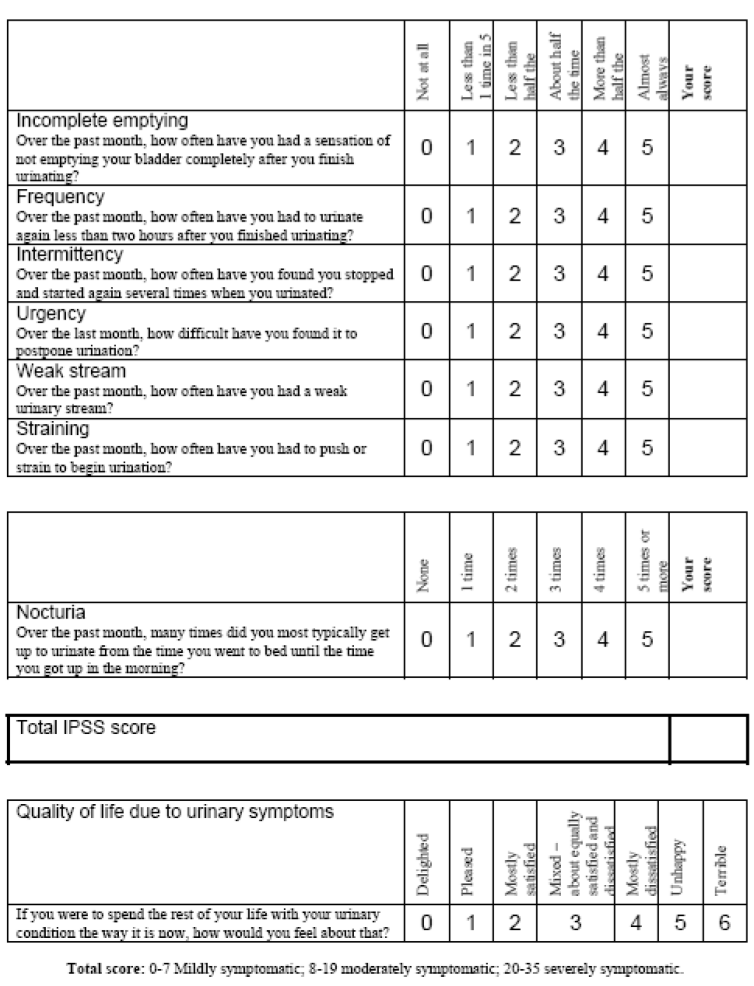
Fig 1. IPSS is a questionnaire to determine the severity of the prostate symptoms
2. Physical examination [Fig 2]. The abdomen is examined for any bladder distension and a rectal exam (DRE) done to feel the consistency of the prostate and estimate its size. The DRE is also helpful in detecting any hard prostate nodule that may indicate cancer.
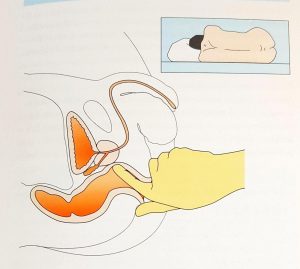
Fig 2. Digital rectal exam (DRE) is done to assess the prostate size and shape
3. Prostate Specific Antigen (PSA). This is a blood test to detect prostate cancer. It should not exceed 4 ug/L. If so, prostate cancer must be excluded through transrectal ultrasound guided biopsy (TRUS/bx).
4. Ultrasound [Fig 3]. Ultrasound can assess the prostate shape, prostate size, and determine the post-void residual urine volume [3a]. A prostate size of > 20 ml and residual urine of > 100 ml is considered as abnormal. Ultrasound can also assess the kidneys to see if they are blocked (hydronephrosis) [3b].
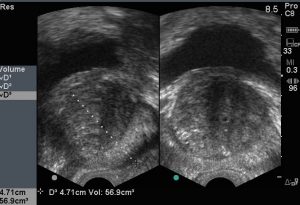
Fig 3a. Ultrasound to measure the prostate size and residual volume in the bladder

Fig 3b. Ultrasound showing hydronephrosis of both kidneys from severe BPH
5. Uroflow [Fig 4]. The uroflow is a dynamic test that measures the speed of urination. A transducer in the machine records and translates the flow into a graph to give a good visual indicator to the degree of bladder blockage. A normal flow will show as a bell-shaped curve [4a], while an obstructed bladder will show a strained, slow pattern [4b].

Fig 4. Uroflow machine is used to measure the speed of urination
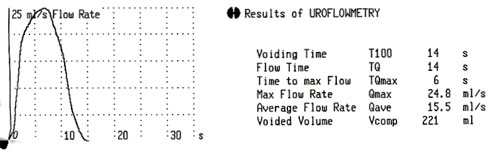
a) normal uroflow pattern
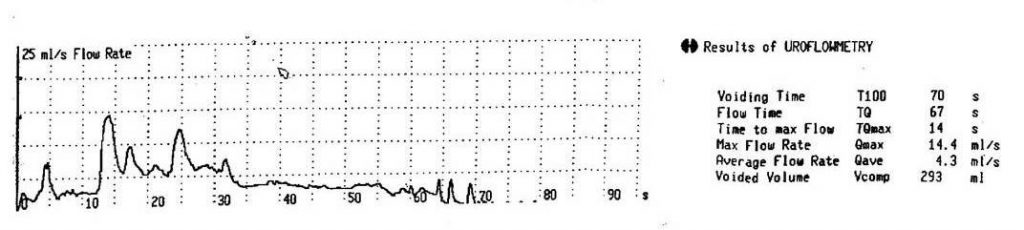
b) obstructed uroflow pattern
Complications [Fig 5]
BPH can be a progressive disease. Left untreated, there is a risk of significant bladder blockage leading to high residual urine, which in turn can lead to repeated urinary infection and formation of bladder diverticuli / stone. As the blockage gets worse, chronic retention of urine and swelling of the kidneys (hydronephrosis) can occur to cause kidney failure [5a]. Ultimately, sudden painful inability to pass urine occurs to cause acute retention of urine [5b].
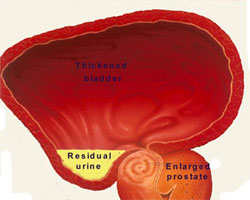
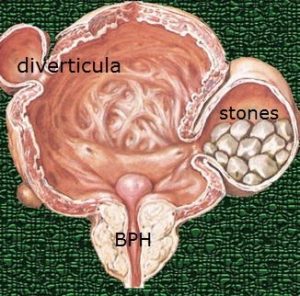
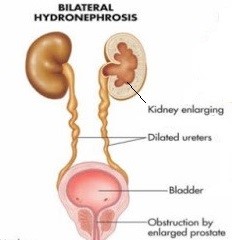
Fig 5a. Complications of BPH: residual urine, diverticuli, stone formation & ultimately, hydronephrosis
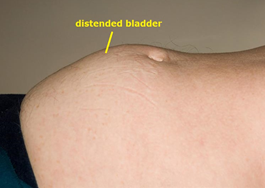
Fig 5b. acute retention of urine from BPH
Treatment
a) Medication [Fig 6]
Medical therapy is the first-line treatment. There are 2 main groups of drugs available. The first are the alpha1-blockers, (e.g. Hytrin, Xatral, Harnal) which relax the tone of the prostate and bladder neck. They are 70% effective, but carry a 10% risk of giddiness due to lowering of the blood pressure. However, they do nothing to reduce the prostate size. The second group are the 5-alpha reductase inhibitors, (e.g. Proscar, Avodart) which block the action of the male hormone, dihydrotestosterone (DHT) on the prostate, thereby decreasing prostate size. They are indicated for large glands (> 30 ml size) but can take up to 3 months to sufficiently reduce the prostate size. Hence, combination with alpha1-blocker is needed for the initial months. A dual drug, Duodart (Harnal + Avodart) is also available as a single tablet to make dosing convenient.
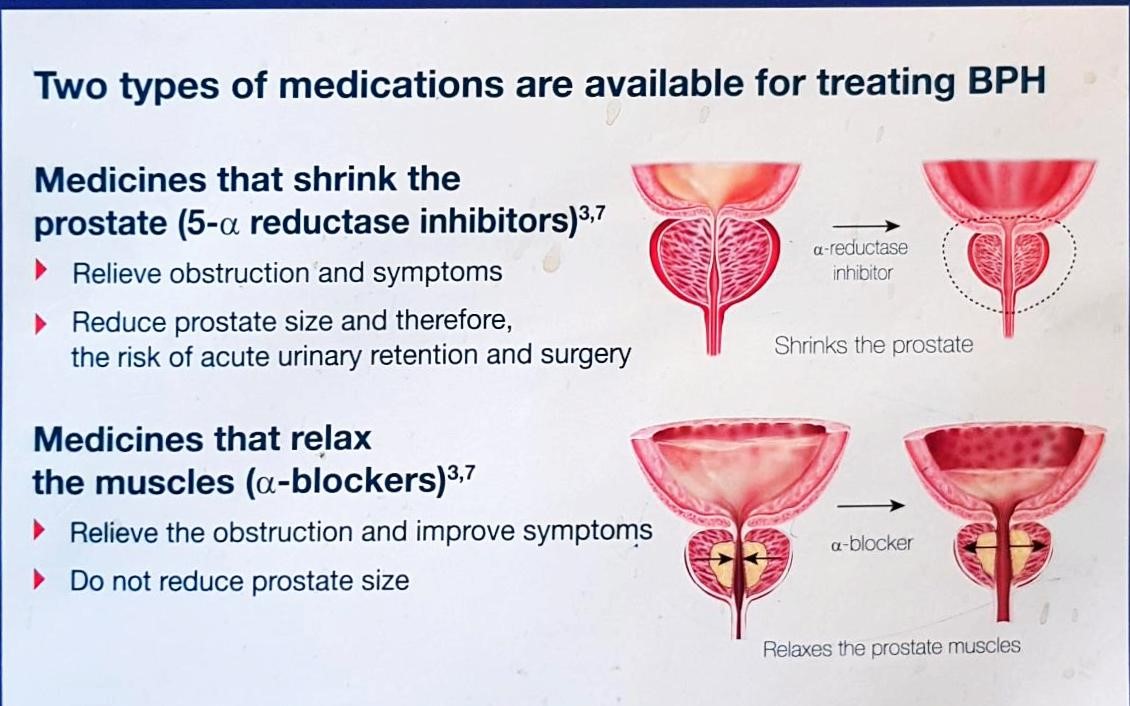
Fig 6. The 2 types of drugs for BPH
b) Surgery [Fig 7]
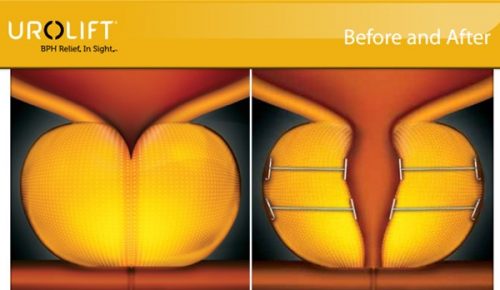
Surgery is indicated when complications arise or when medical treatment fail. The most effective surgery is TURP, which is endoscopic resection of the BPH to recreate an open channel [7a]. It is done under general or spinal anaesthesia and takes 1 hour to do. Hospital stay is 3 to 4 days; the main complications being bleeding and dry ejaculation. There are many variants to TURP, e.g. enucleation TURP, laser TURP but they are essentially different techniques achieving the same outcome of immediate channel creation. The most well-known laser, Greenlight (PVP) laser has the advantage of less bleeding and shorter hospital stay [7b]. However, it is slower to perform and costs more than the standard TURP. Thermotherapy (using heat or steam) [7c] and Urolift (using wires to pull apart the prostate lobes) [7d] are alternative lesser-invasive options but the concern is that their results may not be durable resulting in re-surgery in later years. Open prostatectomy is reserved for very huge BPH > 100 ml and rarely done nowadays.
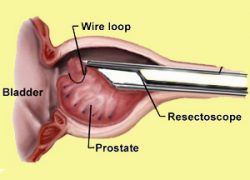
a) Standard TURP
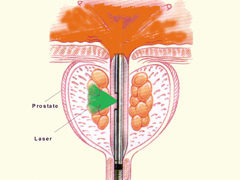
b) PVP
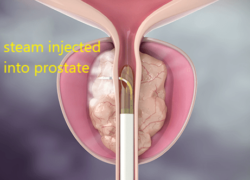
c) Rezum
d) Urolift
Fig 7. Surgery for BPH a)TURP uses a resectoscope to cut away prostate tissue b) Greenlight laser to vaporize prostate tissue c) Rezum uses steam to “melt” the prostate d) Urolift uses wires to pull the lobes apart
Following prostate surgery, men may still continue to have frequent urination and urgency but this settles by 3 months in 70% of cases. Those who do not resolve have an overactive bladder related to ageing or diabetes which can be controlled with medication. (see article on overactive bladder)