Persistent Prostatitis
Prostatitis is a common cause of pelvic/groin/scrotal pain in men. It can also cause pain during urination similar to urinary tract infection (UTI). Prostatitis is always assumed to be bacterial in origin. Quinolone antibiotics eg. ciprofloxacin and levofloxacin are the commonly prescribed but it may take at least 3 to 4 weeks to eradicate the infection.
Despite giving an adequate course of antibiotics, prostatitis can be frustratingly persistent. In such a situation, underlying causes need to be excluded.
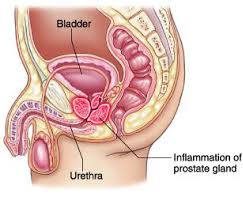
In older men (above 50 years), benign enlargement of the prostate (BPH) can be the source of persistent prostatitis [Fig 1]. Young men (20 to 50 years) are similarly prone to prostatitis. Many of them are assumed to have simple UTI and given a short course of antibiotics which is not sufficient in eradicating all the bacteria within the prostate. They subsequently get a re-infection.
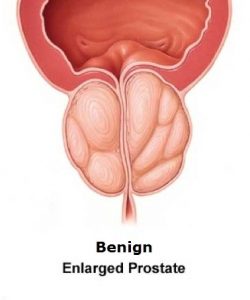
Fig 1. Benign prostate enlargement as a cause of prostatitis
Types
Prostatitis can be classified into the following categories:
- acute bacterial prostatitis
- chronic bacterial prostatitis
- nonbacterial prostatitis (to cause prostatodynia and chronic pelvic pain syndrome)
a) Acute bacterial prostatitis (ABP)
The symptoms come on suddenly and include:
- Fever and chills
- Sharp pain in the pelvis, lower back or groin
- Burning pain during urination (dysuria)
- Frequent urination
- Blood in urine
- Difficulty in urination and even painful retention of urine
The prostate will feel boggy and very tender [Fig 2]. The urine will usually be positive for bacteria and the prostate specific antigen (PSA) level elevated. ABP requires intravenous antibiotics until the fever subsides, followed by oral antibiotics for at least 3 weeks. Failure to continue antibiotics for an adequate duration can lead to recurrent bacterial prostatitis.
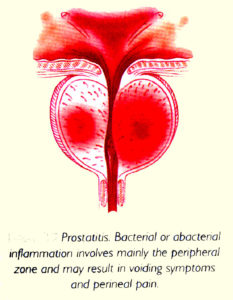
Fig 2. Acute prostatitis
b) Chronic bacterial prostatitis (CBP)
Chronic bacterial prostatitis develops more slowly and usually does not cause high fever. Other symptoms are:
- Frequent and urgent need to urinate, both day and night
- Dull ache in the pelvic area, inner thigh, lower back and scrotum
- Pain referred to the penis tip at the end of micturition
- Blood in urine or semen
- Pain after ejaculation
CBP is often diagnosed late because the symptoms tend to wax and wane. Another reason is incompletely treated ABP. On examination, the prostate feels indurated and tender, sometimes even nodular to simulate prostate cancer [Fig 3]. To compound matters, the PSA level is often elevated and lead to prostate biopsies. A longer course of antibiotics up to 3 months may be needed to adequately eradicate resistant cases of CBP. Atypical bacteria like mycoplasma may also account for why some cases do not respond to standard antibiotics.
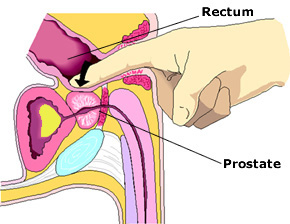
Fig 3. Digital prostate examination may reveal an indurated / tender prostate
c) Chronic non-bacterial prostatitis
Chronic non-bacterial prostatitis is a persistent non-infective inflammation of the prostate. The symptoms are similar to those of chronic bacterial prostatitis, so a diagnosis of non-bacterial prostatitis is made only after an adequate course of antibiotics has been given. Also, as bacteria can easily become resistant to common antibiotics, the only way to prove whether there is still a bacterial cause is to culture the semen.
Nonbacterial prostatitis may also be chemical in nature, e.g. from reflux of urine into the prostate as a result of an overactive urinary sphincter caused by mental stress, habit of holding the bladder and excess caffeine. Non-steroidal anti-inflammatory drugs (NSAIDs) and alpha-blockers are commonly used to relieve this type of prostatitis.