Robotic/Laparoscopic Adrenalectomy
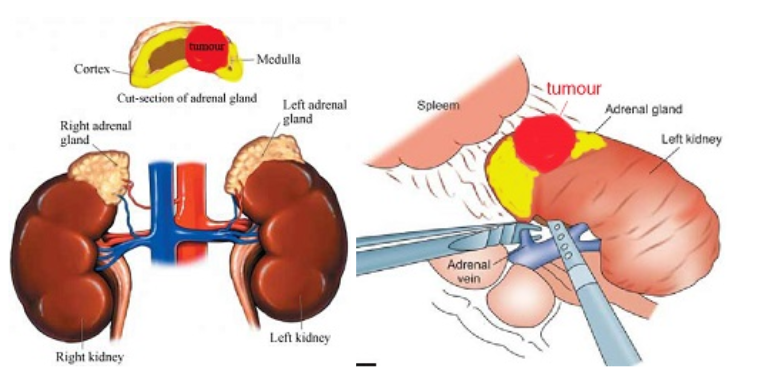
Adrenal tumours are rare but can be the cause of hypertension by producing excess hormones. These patients report excess sweating, palpitations, weight gain, headaches and water retention. These “functional” tumours include pheochromocytoma, Conn’s syndrome, Cushing’s tumour and adrenal cancer. Adrenal tumours may also be non-functional and cause no symptoms; these are picked up from incidental screening. This include adrenal adenoma and angiomyolipoma. For patients diagnosed with small adrenal tumours less than 6 cm, they no longer need open surgery to remove them. Laparoscopic and robotic adrenalectomy are minimally invasive techniques that can now be done safely with faster recovery. These keyhole approaches have the advantage of less bleeding, less pain, smaller scars and shorter hospital stay.
How it is done
Under general anaesthesia, the patient is placed in a lateral position and pressure points are padded. A camera port is inserted, abdomen distended with gas and two working ports are then inserted under direct vision. The adrenal gland is exposed and all the blood vessels supplying it are sealed with diathermy or energy-sealing device. The whole gland and tumour is placed in a plastic bag and extracted at the end of the surgery.
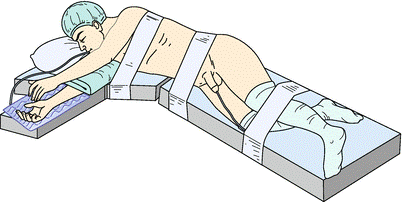
Patient position for laparoscopic / robotic adrenal surgery

Robotic arms in position
The robotic method has the additional advantage of making the surgery even safer (less blood loss, lower conversion rate) through its superior 3-dimensional, 10-times magnified vision and dextrous instruments. The surgery takes 2 to 3 hours for standard laparoscopic method, but shorter (as fast as 1 hour) for robotic method. Hospital stay is 1 to 2 days.

Dr Chin performing robotic adrenalectomy on Si robot
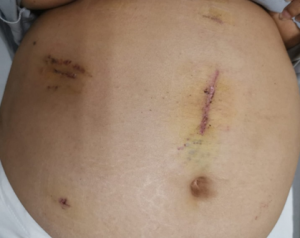
Scars from robotic right adrenalectomy for a 8.5 cm adrenal angiomyolipoma in a 78 kg woman
Complications include:
- bleeding. Blood loss is generally low (< 100 ml)
- blood pressure fluctuations. This applies to functional tumours, especially pheochromocytoma and Conn’s syndrome, where a sudden drop in blood pressure can occur once the adrenal vein is ligated. In addition, for pheochromocytoma, the blood pressure can rise to dangerous levels when handling of the tumour. Such fluctuations in blood pressure can cause major strokes and heart attacks.
- conversion. As with all laparoscopic techniques, conversion to open surgery is always possible if excess difficulty or bleeding is encountered. The conversion rate is much lower with robotic method.
- adjacent organ injury. As the adrenal gland is located in a tight space, organs adjacent to it may be injured during the dissection. E.g. pancreas and spleen on the left side; duodenum and liver on the right side.
Desired outcomes:
- no blood transfusion ( < 1% of cases )
- no excessive blood pressure changes
- no conversion to open surgery ( < 4% chance )